Involving and engaging carers in research
Report from a webinar on 6 June 2022 hosted by the NIHR Centre for Engagement and Dissemination and the NIHR School for Social Care Research
Published Nov 2022
Report from a webinar on 6 June 2022 hosted by the NIHR Centre for Engagement and Dissemination and the NIHR School for Social Care Research
Published Nov 2022
This report has been co-authored by Peter Atkins, Dave Martin, Margaret Ogden and Yasma Osman drawing from their talks at the 6 June 2022 webinar, supported by Sophie Jarvis and Anji Mehta.
Bryher Bowness (King’s College London) and Yasma have authored a section of this report providing context from their ongoing research, also based on their talk at a webinar on 6 June 2022.
Martin Knapp (NIHR SSCR) and Jeremy Taylor (NIHR CED) have provided reflections on the key messages from the report and webinar.
Editorial support was provided by Mike Horn.
We know that many “carers” would not identify as being a carer or do not prefer this term.
Throughout this report we use the term “carer” to talk about people who are providing unpaid carer to a family member, partner and/or friend.
We refer to ‘PPI’ for ‘patient and public involvement’ in places and know this is not a term used in social care; it is used in places for ease and represents all involvement.
NIHR School for Social Care Research (2022) Involving and Engaging Carers in Research: Report from a Webinar on 6 June 2022, NIHR School for Social Care Research, London.
We are a group of individuals with our own unique experiences of caring for our loved ones. Some of us would call ourselves ‘carers’ and others wouldn’t use this term. Some of us have cared for family members in their final years, and some have supported our partners or siblings over many years. Our lives are linked to those we care for; impacts on the care and support they receive will impact us and vice versa.
As carers we are an integral part of the care process and are extremely well versed in the conditions and needs of the people we care/have cared for. We may not be formally identified as part of the care workforce, but unpaid family carers are a large – even if sometimes hidden – part of the system of support for people using health and/or care services.
We believe that research should lead to improvements in the way care and support is organised and delivered. Good research will include the voices of people using health and care services, carers, and health and social care professionals.
All of us have a deep understanding of what it means to be a carer and the variety of support this can include. This intimate understanding of the daily issues people with care needs face is an important resource for researchers; we believe involving carers at the beginning of research has a beneficial impact on the direction and impact of a study.
Yet we are not just defined by our caring roles in the lives of people using health and care services; we are also individuals with our own needs and distinct experiences. Research does not always capture the carer’s perspective on health and social care support or ensure it captures the impact on carers of any intervention or support provided for the person they care for. It is extremely important not to forget the needs of, and support required, by carers themselves.
Our experiences mean we have important insights that are valuable for research. We have been involved in research projects in different ways.
Our experiences of research have generally been positive, and many good things have come from our involvement in different projects. We believe in the projects we participate in and hope they will improve the wellbeing and mental and physical health of carers and those they care for, as well as improving how research is designed and carried out.
But more needs to be done to tap into the valuable insights that carers can provide to research.
We believe that increasing co-production, co-researching and inviting carers to share their vision about the kind of care and support we want for our loved ones should be important to those funding and carrying out research.
Many of you reading this report will have looked after a loved one or been looked after by your family or friends, even if just for a short time. You may already be involved in research or thinking about getting involved. It is our hope that this report will provide the beginnings of a road map for the deeper involvement of carers in research, which will result in whole system improvements for care and support and improved outcomes for us and others in our position, and the loved ones we all care for.
Peter, Dave, Margaret, Yasma
Carers (known as unpaid or family carers) play an invaluable role in society. They have a variety of experiences and expertise in the needs of the person or people they care for or have cared for as well as their own experiences of being carers. Their individual voices are important in health and social care research, yet they are often not involved or engaged in shaping or supporting research.
More research is needed on the role, needs and support for carers. But the voice of carers also needs to be captured in both shaping and carrying out all health and social care studies even when the focus is on the cared-for person.
As part of Carers Week 2022, the NIHR Centre for Engagement and Dissemination and the NIHR School for Social Care Research jointly organised a webinar to explore the experiences of (unpaid) carers involved in health and social care research.
The webinar brought together carers engaged in research funded by the National Institute of Health and Care Research (NIHR) to explore our experiences, and to hear our suggestions on how to improve the involvement and engagement of carers in research.
The webinar included a presentation from Bryher Bowness (PhD student at King’s College London) on initial findings from a systematic review looking into involvement of carers in research, exploring the methods and outcomes of working with carers to conduct health and social care research.
Jeremy Taylor (NIHR Director for Public Voice and Director of the NIHR Centre for Engagement and Dissemination) shared his reflections in the webinar too.
This report summarises our talks during the webinar and suggestions from the audience.
The webinar is part of a programme of work that NIHR CED and SSCR will support on carers involvement, led by a working group of carers involved across NIHR-funded research.
I am a PhD student at King’s College London and have been working with Yasma Osman on research around the involvement of carers. I presented emerging findings from my research at the 6 June webinar.
Involvement is known by different terms, such as ‘PPI’ (public and patient involvement), participation, engagement but broadly involvement is about working together with people who are affected by the research within the research process, not just as research participants.
There are different levels of involvement:
There has been a lot of literature looking at general patient and public involvement in research, but carers are often either left out of this or included within a focus on “service users”.
This does not recognise the important contribution carers have to make, both in terms of the needs of the person they care for and their own health and care needs.
Carers will also have different motivations for getting involved in research and different needs during the research, and the literature does not reflect this.
As part of my PhD research I will be working collaboratively with carers, and although there was a lot of advice that came from sort of single case studies about how to do this, there was no evidence-based approach on how best to involve carers in the research.
So, I carried out a systematic review on the methods and outcomes of working with carers to conduct research. The review included journal articles and unpublished literature, and I only included literature where the majority of the public involved in the study were carers of all different conditions.
I found 43 studies where carers were involved in studies – an increase from the handful of unpublished studies found in 2007 by Repper and colleagues. The studies varied a lot with some qualitative studies and some randomised controlled trials. There were lots of different conditions covered, including carers of people living with dementia, palliative care, paediatric illnesses and mental health needs among others.
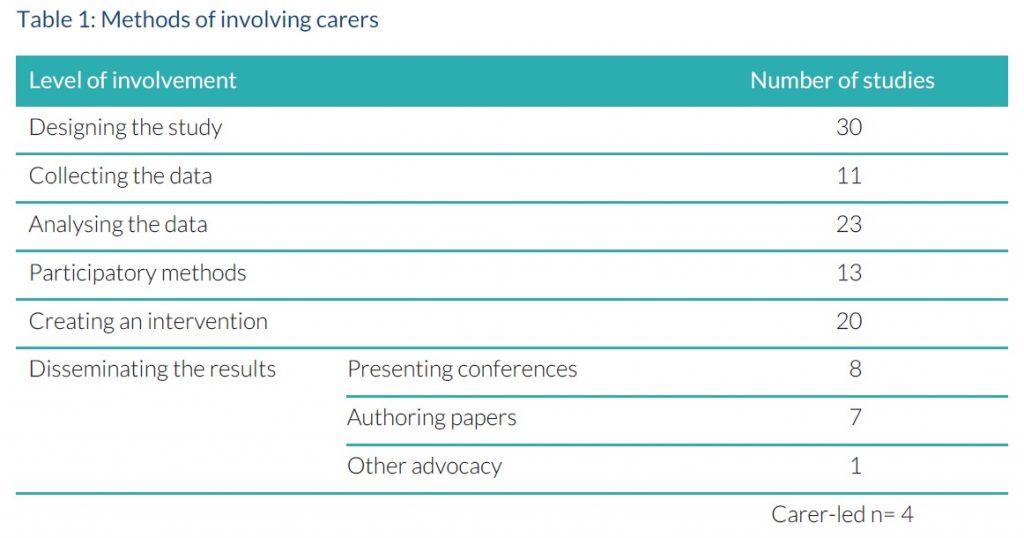
Table 1 shows the different methods of involving carers in the studies I found. The majority of studies involved carers in the design of the research and analyses. There were a lot of different examples of how carers were involved in dissemination through creating their own blogs or films.
A key conclusion from the research is that there is no “one size fits all” approach to involving carers in research. Different studies have different questions and need to use different methods based on the varying needs of the carers involvement. Methods need be constantly evaluated and adapted throughout the course of research based on how things are working and feedback from the carers involved on their experiences.
Key messages on the best ways to include carers so far include:
I am currently completing analyses and will write up the full paper soon. I have found a lot of ‘conference abstracts’ in the search results where studies talked about their involvement but haven’t written this into a paper. I was surprised by the number of research projects that did involve carers but didn’t write about this in detail in the papers because there wasn’t space to do that – they would have needed to write a whole separate paper. There’s still a long way to go.
My personal experience of involvement in my research has reflected many of the barriers identified in the literature, including long processing times within the institution. My key takeaways have been to:
Involvement of carers in research is not only important for the research and for their carers but can be a very beneficial experience for the researchers too: I have definitely found Yasma to be a source of inspiration and someone who has enthused me to carry on with the research.
At the webinar we spoke about our experiences. People attending the webinar also shared their suggestions.
I am a mother, grandmother, family social carer. I am British Somalia which means I am a very diverse character. I am involved in Bryher’s project and also the Recollect and Recovery College.
The reason I got involved in Bryher’s project and other projects is because my brother is even more diverse than I am, and I have found major negative issues being Black, well-educated and well-spoken, both within the mental health field and in any field to be honest with you. I think people assume things about you – that you’re loud and aggressive – and don’t treat you in the same way as others.
So, I’m in research for my big brother who has lived with schizophrenia for almost fifty years. He lives in a care home, and I believe that the residents in mental health care homes are not getting what they should be getting, both from a diverse cultural aspect (e.g. food, social well- being) and in support for their mental health wellbeing.
I am involved in these projects as a carer because I believe that the research is going somewhere, and I believe that my time should be spent – on my brother’s behalf – to help diversity, inclusivity and mental health and wellbeing for all to move forward. I think that Bryher’s project is what this is all about; if it wasn’t I wouldn’t be involved.
One of the negative aspects I found with the projects I am involved in is the use of jargon. I am very well educated, I’ve travelled the world and studied everything but sometimes the research jargon does get me a little bit bogged under.
I am mental health carer and look after somebody with borderline personality disorder since 1990. I also set up and ran a mental health carers charity in Dorset which started in 2004 until 2013 and we represented about 150 mental health carers – I’m drawing on their experiences as well as my own.
I also work at Bournemouth University as one of the BU PIER Officers in public involvement in education research; the programmes I work in are social work, occupational therapy, paramedic science, physiotherapy and operating department practice so I get to hear students talking about their placements which is very rewarding.
I got involved at Bournemouth University in a research project in 2017/18 which was interviewing 11 older male carers so all of them 80 years old and above with half from Bournemouth and half from Poole. We split the interviewing between the team and I interviewed three carers in their homes; those interviews came out with a wealth of information on what was working and what wasn’t. From the project we produced a journal paper published in the Journal of Community Nursing in 2017/18, and a video (Bournemouth University, Chief Cook and Bottle Washer) which won an award in Dorset. Most people who watch the video are really touched by the evidence the carers give.
Another thing that came out of the project was that we set up a male carers support group in a local GP surgery which we hadn’t planned, and we received funding for a leaflet that went to all of the GP surgeries in Dorset talking about the issues for older male carers to help provide support.
That sort of lit the fire for me as the research had been really useful especially as we did this in the 3–4 month period. It was a small project which had quite a big impact.
I then decided to link up with the NIHR Policy Research Unit in Adult Social Care (ASCRU) in 2019 as a member of their public involvement and engagement group. I got involved in a project through ASCRU on strengths-based approaches to social work and care. In the project I contributed to a final version of a report which is currently in draft form and a literature review which was published as a journal paper. I felt really valuable as part of the ASCRU project and was listened to.
It’s OK to say ‘no’ as a carer asked to join a research project. I know that sounds strange, but I would advise not over committing and not to agree to join a project unless you’re happy with it and you understand what’s required of you because I see that happening a lot. Make sure you are clear what’s required from you.
Don’t be afraid to ask about payment. It’s not a dirty word – some people don’t want to be paid but others do – and it’s important to know.
Don’t send last-minute requests – it’s not good.
Make sure you have good communication and keep the carers informed through the research process.
Payment details are really important, and timescales for processing.
Don’t use the same person all the time across different projects. New people need support to develop and opportunities to get involved too.
It’s always important to find out how long someone’s been a carer because if you’ve got somebody who has been looking after someone with a condition for a while, they’re extremely well-versed in it. They probably know the situation better than the researcher they’re talking to. There are some of the carers that are really experienced and engaged, and some who have never done it before. That’s why the initial conversation with the researcher is really important, to find out what the opportunities are and how the carer feels.
Useful links
VOICE is a unique organisation which supports involvement: https://www.voice-global.org.
In Bournemouth University we have just started a PPI course for researchers which is being run twice a year: https://www.applycpd.com/BU/courses/112131.
I am a public advisor in research and have been a carer three times: first for my gran, second for my mother who had cancer and, thirdly, for my uncle. I do think caring for them has been a privilege, as well as trying to help them. I do think I have learned an awful lot about me, I’ve developed new skills. At times it’s been hard, particularly when I got diagnosed with an illness myself, I did find caring quite difficult, but I was determined to carry on with the role.
I think ‘PPI’ is very different from a carer’s perspective, and quite often I find myself just sort of thinking; will my uncle be comfortable with me sharing this with researchers and other PPI members?
Before he got dementia I could actually ask him: I could say, what do you think about this? How was your care this week? Then I could relay it back word-for-word. However, when his dementia developed that was quite difficult. I had to make my own judgements about what I was going to share about his care, both in his domestic home when it was me and a professional carer looking after him, and also in a care home in the last two years.
So it was also about sensitive topics, what do I reveal about this? Talking about his personal relationships would have been off limits for me as that was part of his private life. However, there were other things socially that he did, like his voluntary military contribution and the work that he did with the family history group – those kind of things I would share, and also things to do with nutrition, mobility and the different aspects of his condition. It would be helpful to have guidance about this, and having opportunities to have one- to-one conversations with a research colleague or a public involvement member about situations as they come up would be very helpful.
My journey into social care, it came from health and public health when I finally realized there was something missing, and I should do social care, and I must say I feel I have been very welcomed into the social care field. I joined the NIHR School for Social Care Research’s public involvement group in 2019 and have been involved in two projects so far.
The first is on NICE guidance. It’s never been done before, but London School of Economics and Political Science is doing a project on looking at the implementation of NICE’s social care guidance. I am co-chair of the national involvement group. Another project was on resilience and recovery post-covid. That project was really exciting as it was international. I remember doing a workshop where we had a big virtual mural, and we imported and populated the mural with information. This was my first project and the negative side of that was I jumped straight into social care on a very high-profile project, and in hindsight perhaps I shouldn’t have done that. I was so well supported by the team, and another member even helped me over the weekend while I was doing the preparation.
I would suggest that training is made available, and that carers joining research projects ask for it – I’m sure the organisations involved will try and help with any training requested.
There are things we’ve developed in health which might be useful, particularly bursaries, going on training courses (more intense training), and also training on how to evaluate involvement. Also awards, as that’s something we do in health, so occasionally public involvement members are lucky enough to get an award. So that may be something else that the social care research field could learn from the health field.
I have been my sister’s carer since 2014. She has dementia. I say I’m her carer but I’m more a kind of care administrator and manager – I don’t live with her nor administer personal care; I have power of attorney and have oversight of her care and I guess I provide social and emotional care. For the last 25 years I’ve been involved with what we laughingly call the age sector or the age space, or space age people! Both on a local government level and national level, I’ve been seeking to improve quality of life for older people. So for a number of years, I’ve been a member of the Service User and Carer Advisory Group for the NIHR Health and Social Care Workforce Research Unit at King’s College London and have taken part in a number of research activities since then.
My experience of being involved with research has been extremely positive. The groups I have worked with anticipated and prepared for issues that might arise during the course of the research that could be extremely sensitive or actually quite traumatic for the carers involved in the research, and have prepared for that and provided reassurance.
Researchers need to be very clear about the purpose of involving carers in their project. From the point of the view of the carer this will help them to set boundaries.
People don’t necessarily identify or view themselves as a carer. I might ask myself ‘am I a carer or a partner?’. The number of times I’ve heard somebody say “I’m not a carer, I’ve been her husband for 40 years”, and I think that’s quite an issue to try and sort through, because there’s quite a lot of resistance there. The caring role – is it a job or duty? I think that’s often conflicted in many people’s minds about how to then get involved or see the perspective there. I think there’s a real difficulty in stepping back and contributing the carer’s perspective, rather than the tendency to see involvement as more about improving the cared for person’s circumstances. It’s important to skim away the layers within this.
It’s important to seek to involve people who used to be called ‘hard-to-reach’, and members of diverse communities, particularly culturally marginalized members of communities. It might be useful to talk to trusted points of contact and intermediaries such as community leaders cultural leaders faith groups etc about the nature of ‘caring’ before trying to recruit through the usual referral connections in terms of carers groups and professionals.
Perhaps we should look at the methodology of research to improve involvement which has been touched on by others: approaches such as storytelling for carers experiences, recording over time, using carers’ diaries, buddying, new uses of technology.
And what about incentives? What do I, the carer, get out of taking part? How does it improve things either for my situation or the cared for person? Perhaps not so much about payment BUT other ways to acknowledge the participation and contributions to improving care – vouchers? Reduced council tax? Time banks, reciprocal contract for support?
Something I feel quite strongly about is involving carers at the very beginning. When we’re talking about co-production and co-researching, I think what we should be engaging with carers to design the research questions and, so not just co- designing the research but getting to the nuggets of what the carers are interested in.
The thing I really have to emphasize, though, is it still seems to me that there is still a very much a non-joined up approach to care; professionals are one, unpaid family carers are another. There is no sense of intertwining, and carers are still acknowledged as the Cinderellas, sort of busying around in the shadows. We simply compartmentalize that and reinforce that by focusing upon carers. Why don’t we take far more of a whole system appreciative inquiry approach to understanding the interplay of parts of the care system; an illness, condition impacts way beyond the person themselves but we still seem to have a traditional focus to “treat the liver in bed 9” – and sort of accommodate the family carer as an add on to the cared-for person’s health needs.
So, let’s have more co-production and more co- researching, and invite people in the community to share their vision on the kind of care and support we would want for our loved ones and for ourselves. More vision, please.
A number of useful points were made by participants at the webinar:
Suggestions were made to support improved involvement in research:
Involving carers in research – if done right – will significantly improve the quality and outcomes from research. It will also support those carers to develop their own skills and value the contribution they are making to research that should have the potential to improve lives.
It is important to remember that there is no one size fits all approach to involving carers in research. But there are several points to consider.
An obvious, though frequently missed, factor is that it is beneficial to involve carers from the beginning of research, and this begins with a blank page. Carers should be co-designing the research questions and researchers should be getting to the nuggets of what carers are interested in, rather than involving carers to provide inputs to pre-determined research questions.
Outreach is a vital part of recruitment of carers for involvement activities, and researchers need to consider how to seek to identify and engage with individuals who may not see themselves as a carer, as well as carers from diverse communities and settings. This could also include carers who are homeless, or from the travelling community or faith groups that are outside the system.
It is important to continue to bring in new individuals to support research and develop their skills, rather than just asking the same individuals to join new research projects. This is not only to help carers manage their commitments across projects but also to support carers new to research to develop as well and bring in new perspectives.
Researchers need to communicate the purpose of the research to carers. This will help carers set boundaries about their participation and manage expectations; a written contract or agreement could be useful to set out what they can expect from their participation in a project, including a ‘rights’ checklist which lays out payment details, along with any training and support that could be provided.
It is also important for researchers to clarify whether they are seeking the involvement of a carer in a project as a carer themself, on behalf of a cared for person; or both. PPI is very different from a carer’s perspective. It is important to offer guidance on ethics and confidentiality so that the carer is comfortable with what they share about themselves and the person they care for.
Researchers would benefit from examining their methodology and exploring innovative ways to enable carers to take part in research. This will help minimise carers time or commitment to a project. For example, this could include the way in which technology is used to support involvement, offering meetings outside of traditional research hours, being clear on the minimum time that will be provided with requests, keeping carers informed throughout the research process.
Researchers should ask carers about what they might need to take part in the research as early as possible and make sure the requested support is available. For example, this might be training they would find useful or communication approaches that work better for them.
Finally, a step forward could be conducting research that aims to improve a cared for person’s care as part of a complete system, and in doing so involve all relevant voices without separating carers from professionals and so on.
Health and social care research funded by the National Institute for Health and Care Research (NIHR) has a long history of user, carer and public involvement; the contribution made by many individuals continues to be greatly valued.
We recognise that the voice of unpaid family carers can sometimes be under-represented, however.
We were therefore pleased to host the webinar on 6 June, particularly to engage with Peter, Margaret, Dave and Yasma in sharing their experiences. The presentation from Bryher provided very useful context, and some of the emerging findings from her review will be familiar to many.
In some areas the experiences of carers involved in research mirrors feedback from people involved in research as patients or service users themselves: the importance of simple, fast payment; the need for clear roles; the importance of boundary-setting and clear communication; avoiding jargon; ensuring diversity and inclusion; the need for varied methodologies.
In other areas, getting involved in research is a unique experience for carers. There is the contested question of what it means to be a carer; whether you are there to speak for yourself or on behalf of the person you care for and how much / little you should reveal about the cared-for person. There is perhaps a need for clearer guidance to be developed around these key questions, for the benefit of both carers and researchers.
The webinar has reinforced our sense of what we need to do to strengthen the involvement of carers in research and to improve carers’ experiences of this involvement. We are committed to working with carers to take this forward.
We would like to thank everyone involved in the webinar, particularly Peter, Margaret, Dave, Yasma and Bryher, for taking these discussions forward, their ongoing engagement and commitment to ensuring the inclusion of carers in research becomes standard practice.
NIHR School for Social Care Research
London School of Economics and Political Science Houghton Street
London
WC2A 2AE
Email: sscr@lse.ac.uk
Tel: 020-7955-6238
Web: www.sscr.nihr.ac.uk
Twitter: @NIHRSSCR
© NIHR SSCR, 2022
The NIHR School for Social Care Research is funded by the National Institute for Health and Care Research. www.nihr.ac.uk